Your child’s pediatrician is your best resource for information about your child’s condition. Their individual outlook can vary depending on the condition’s severity, symptoms, and any complications that result.
Many children affected by Canavan disease develop disabilities resulting from issues with their central nervous system.
These complications can have an impact on life expectancy. Many children with Canavan disease don’t reach adolescence.
There is a mild form of Canavan disease that leads to developmental delays and some other symptoms. Though less common than other forms of the disease, children with this mild type of Canavan disease can often live well into adulthood.
Symptoms
The symptoms of the disease can vary greatly. Children affected by the condition may not share the same symptoms.
- Some of the most common symptoms are:
- larger-than-normal head circumference
- poor head and neck control
- reduced visual responsiveness and tracking
- unusual muscle tone, leading to stiffness or floppiness
- unusual posture, with legs often kept straight and arms flexed
- difficulty eating, with food sometimes flowing up into the nose
- difficulty sleeping
- seizures
An increase in head circumference typically develops abruptly. Other symptoms develop more slowly. For example, vision problems may become more obvious as a baby’s development slows down.
Canavan disease is a progressive condition, meaning its symptoms can worsen over time.
complications
Depending on the severity of their condition, children with Canavan disease usually can’t sit up, crawl, or walk. They may also have trouble swallowing.
Children with Canavan disease also experience delayed development. Language and other skills typically come later, if at all. Hearing may or may not be affected by Canavan disease.
These complications can have a direct impact on a child’s quality of life.
causes and risk factors
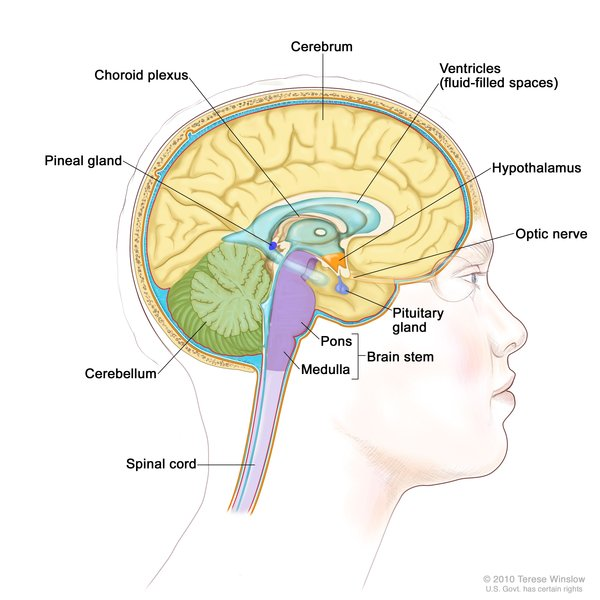
Canavan disease is one of several genetic disorders known as leukodystrophies. These conditions affect the myelin sheath, the thin coating around nerves. Myelin also helps transmit signals from one nerve to another.
Children affected by this condition lack an important enzyme called aspartoacylase (ASPA). This natural chemical helps break N-acetylaspartic acid down into the building materials that form myelin. Without ASPA, myelin can’t form properly, and nerve activity in the brain and the rest of the central nervous system is affected.
Both parents must carry the defective gene that causes an absence of ASPA in order for their child to develop Canavan disease. When both parents have the gene, each child will have a 25 percent chanceTrusted Source of developing this genetic disorder.
About one in 55 Ashkenazi Jews carry the Canavan disease genetic mutation.
How is this condition diagnosed?
A prenatal blood test can reveal whether the fetus has Canavan disease.
If you carry the Canavan gene mutation, you may want to discuss genetic testing prior to becoming pregnant.
If you’re already pregnant, you may want to have the blood test done to see if your baby has been affected.
What treatment options are available?
There isn’t a cure for Canavan disease. The goal of treatment is to reduce your child’s symptoms and improve their quality of life.
Your child’s treatment plan will vary depending on their individual symptoms. Your child’s pediatrician will work with you and your child to determine how to best meet their needs.
For example, feeding tubes can also be helpful for children who have serious swallowing problems. These tubes can ensure that your child is getting all of the nutrients they need and enough fluids to stay hydrated.
Physical therapy and adaptive equipment may be helpful in promoting better posture. Lithium or other medications may be helpful in controlling seizures.
Where to find support
To help you and child cope with Canavan disease, find a regional or online support group. The Canavan Disease Patient Insight Network is an online resource to help families learn about research and promising treatments. The group also serves as a way to connect with a community of families dealing with the same struggle.
There is some encouraging research in treating Canavan disease, but the studiesTrusted Source are in their early stages. Research includes the study of stem cells and gene therapy. A few international registries of Canavan disease are forming to better study causes and possible cures and treatments.
If you’re interested, reach out to the Canavan Disease Patient Insight Network or the Canavan Foundation for more information. You should also have a conversation with your child’s pediatrician about your options and what to expect in the months and years ahead.

Comments
Post a Comment