Overview
Uterine fibroids are noncancerous growths of the uterus that often appear during childbearing years. Also called leiomyomas (lie-o-my-O-muhs) or myomas, uterine fibroids aren't associated with an increased risk of uterine cancer and almost never develop into cancer.
Fibroids range in size from seedlings, undetectable by the human eye, to bulky masses that can distort and enlarge the uterus. You can have a single fibroid or multiple ones. In extreme cases, multiple fibroids can expand the uterus so much that it reaches the rib cage and can add weight.
Many women have uterine fibroids sometime during their lives. But you might not know you have uterine fibroids because they often cause no symptoms. Your doctor may discover fibroids incidentally during a pelvic exam or prenatal ultrasound.
Symptoms
Many women who have fibroids don't have any symptoms. In those that do, symptoms can be influenced by the location, size and number of fibroids.
In women who have symptoms, the most common signs and symptoms of uterine fibroids include:
- Heavy menstrual bleeding
- Menstrual periods lasting more than a week
- Pelvic pressure or pain
- Frequent urination
- Difficulty emptying the bladder
- Constipation
- Backache or leg pains
Rarely, a fibroid can cause acute pain when it outgrows its blood supply, and begins to die.
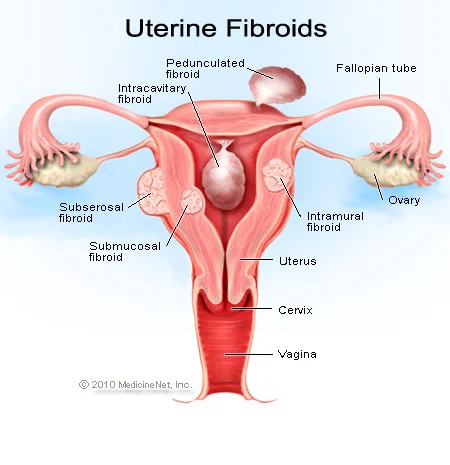
Fibroids are generally classified by their location. Intramural fibroids grow within the muscular uterine wall. Submucosal fibroids bulge into the uterine cavity. Subserosal fibroids project to the outside of the uterus.
When to see a doctor
See your doctor if you have:
- Pelvic pain that doesn't go away
- Overly heavy, prolonged or painful periods
- Spotting or bleeding between periods
- Difficulty emptying your bladder
- Unexplained low red blood cell count (anemia)
Seek prompt medical care if you have severe vaginal bleeding or sharp pelvic pain that comes on suddenly.
Causes
Doctors don't know the cause of uterine fibroids, but research and clinical experience point to these factors:
- Genetic changes. Many fibroids contain changes in genes that differ from those in typical uterine muscle cells.
- Hormones. Estrogen and progesterone, two hormones that stimulate development of the uterine lining during each menstrual cycle in preparation for pregnancy, appear to promote the growth of fibroids.
- Fibroids contain more estrogen and progesterone receptors than typical uterine muscle cells do. Fibroids tend to shrink after menopause due to a decrease in hormone production.
- Other growth factors. Substances that help the body maintain tissues, such as insulin-like growth factor, may affect fibroid growth.
Extracellular matrix (ECM). ECM is the material that makes cells stick together, like mortar between bricks. ECM is increased in fibroids and makes them fibrous. ECM also stores growth factors and causes biologic changes in the cells themselves.
Doctors believe that uterine fibroids develop from a stem cell in the smooth muscular tissue of the uterus (myometrium). A single cell divides repeatedly, eventually creating a firm, rubbery mass distinct from nearby tissue.
The growth patterns of uterine fibroids vary — they may grow slowly or rapidly, or they may remain the same size. Some fibroids go through growth spurts, and some may shrink on their own.
Many fibroids that have been present during pregnancy shrink or disappear after pregnancy, as the uterus goes back to its usual size.
Risk factors
There are few known risk factors for uterine fibroids, other than being a woman of reproductive age. Factors that can have an impact on fibroid development include:
Race. Although all women of reproductive age could develop fibroids, black women are more likely to have fibroids than are women of other racial groups. In addition, black women have fibroids at younger ages, and they're also likely to have more or larger fibroids, along with more-severe symptoms.
Heredity. If your mother or sister had fibroids, you're at increased risk of developing them.
Other factors. Starting your period at an early age; obesity; a vitamin D deficiency; having a diet higher in red meat and lower in green vegetables, fruit and dairy; and drinking alcohol, including beer, appear to increase your risk of developing fibroids.
Complications
Although uterine fibroids usually aren't dangerous, they can cause discomfort and may lead to complications such as a drop in red blood cells (anemia), which causes fatigue, from heavy blood loss. Rarely, a transfusion is needed due to blood loss.
Pregnancy and fibroids
Fibroids usually don't interfere with getting pregnant. However, it's possible that fibroids — especially submucosal fibroids — could cause infertility or pregnancy loss.
Fibroids may also raise the risk of certain pregnancy complications, such as placental abruption, fetal growth restriction and preterm delivery.
Diagnosis
Uterine fibroids are frequently found incidentally during a routine pelvic exam. Your doctor may feel irregularities in the shape of your uterus, suggesting the presence of fibroids.
If you have symptoms of uterine fibroids, your doctor may order these tests:
Ultrasound. If confirmation is needed, your doctor may order an ultrasound. It uses sound waves to get a picture of your uterus to confirm the diagnosis and to map and measure fibroids.
A doctor or technician moves the ultrasound device (transducer) over your abdomen (transabdominal) or places it inside your vagina (transvaginal) to get images of your uterus.
Lab tests. If you have abnormal menstrual bleeding, your doctor may order other tests to investigate potential causes. These might include a complete blood count (CBC) to determine if you have anemia because of chronic blood loss and other blood tests to rule out bleeding disorders or thyroid problems.
Other imaging tests
If traditional ultrasound doesn't provide enough information, your doctor may order other imaging studies, such as:
- Magnetic resonance imaging (MRI). This imaging test can show in more detail the size and location of fibroids, identify different types of tumors, and help determine appropriate treatment options. An MRI is most often used in women with a larger uterus or in women approaching menopause (perimenopause).
- Hysterosonography. Hysterosonography (his-tur-o-suh-NOG-ruh-fee), also called a saline infusion sonogram, uses sterile salt water (saline) to expand the uterine cavity, making it easier to get images of submucosal fibroids and the lining of the uterus in women attempting pregnancy or who have heavy menstrual bleeding.
- Hysterosalpingography. Hysterosalpingography (his-tur-o-sal-ping-GOG-ruh-fee) uses a dye to highlight the uterine cavity and fallopian tubes on X-ray images. Your doctor may recommend it if infertility is a concern. This test can help your doctor determine if your fallopian tubes are open or are blocked and can show some submucosal fibroids.
- Hysteroscopy. For this exam, your doctor inserts a small, lighted telescope called a hysteroscope through your cervix into your uterus. Your doctor then injects saline into your uterus, expanding the uterine cavity and allowing your doctor to examine the walls of your uterus and the openings of your fallopian tubes.
Treatment
There's no single best approach to uterine fibroid treatment — many treatment options exist. If you have symptoms, talk with your doctor about options for symptom relief.
Watchful waiting
Many women with uterine fibroids experience no signs or symptoms, or only mildly annoying signs and symptoms that they can live with. If that's the case for you, watchful waiting could be the best option.
Fibroids aren't cancerous. They rarely interfere with pregnancy. They usually grow slowly — or not at all — and tend to shrink after menopause, when levels of reproductive hormones drop.
Medications
Medications for uterine fibroids target hormones that regulate your menstrual cycle, treating symptoms such as heavy menstrual bleeding and pelvic pressure. They don't eliminate fibroids, but may shrink them. Medications include:
Gonadotropin-releasing hormone (GnRH) agonists. Medications called GnRH agonists treat fibroids by blocking the production of estrogen and progesterone, putting you into a temporary menopause-like state. As a result, menstruation stops, fibroids shrink and anemia often improves.
GnRH agonists include leuprolide (Lupron Depot, Eligard, others), goserelin (Zoladex) and triptorelin (Trelstar, Triptodur Kit).
Many women have significant hot flashes while using GnRH agonists. GnRH agonists typically are used for no more than three to six months because symptoms return when the medication is stopped and long-term use can cause loss of bone.
Your doctor may prescribe a GnRH agonist to shrink the size of your fibroids before a planned surgery or to help transition you to menopause.
Progestin-releasing intrauterine device (IUD). A progestin-releasing IUD can relieve heavy bleeding caused by fibroids. A progestin-releasing IUD provides symptom relief only and doesn't shrink fibroids or make them disappear. It also prevents pregnancy.
Tranexamic acid (Lysteda, Cyklokapron). This nonhormonal medication is taken to ease heavy menstrual periods. It's taken only on heavy bleeding days.
Other medications. Your doctor might recommend other medications. For example, oral contraceptives can help control menstrual bleeding, but they don't reduce fibroid size.
Nonsteroidal anti-inflammatory drugs (NSAIDs), which are not hormonal medications, may be effective in relieving pain related to fibroids, but they don't reduce bleeding caused by fibroids. Your doctor may also suggest that you take vitamins and iron if you have heavy menstrual bleeding and anemia.
Noninvasive procedure
MRI-guided focused ultrasound surgery (FUS) is:
A noninvasive treatment option for uterine fibroids that preserves your uterus, requires no incision and is done on an outpatient basis.
Performed while you're inside an MRI scanner equipped with a high-energy ultrasound transducer for treatment. The images give your doctor the precise location of the uterine fibroids. When the location of the fibroid is targeted, the ultrasound transducer focuses sound waves (sonications) into the fibroid to heat and destroy small areas of fibroid tissue.
Newer technology, so researchers are learning more about the long-term safety and effectiveness. But so far data collected show that FUS for uterine fibroids is safe and effective.
Minimally invasive procedures
Certain procedures can destroy uterine fibroids without actually removing them through surgery. They include:
Uterine artery embolization. Small particles (embolic agents) are injected into the arteries supplying the uterus, cutting off blood flow to fibroids, causing them to shrink and die.
This technique can be effective in shrinking fibroids and relieving the symptoms they cause. Complications may occur if the blood supply to your ovaries or other organs is compromised. However, research shows that complications are similar to surgical fibroid treatments and the risk of transfusion is substantially reduced.
Radiofrequency ablation. In this procedure, radiofrequency energy destroys uterine fibroids and shrinks the blood vessels that feed them. This can be done during a laparoscopic or transcervical procedure. A similar procedure called cryomyolysis freezes the fibroids.
With laparoscopic radiofrequency ablation (Acessa), also called Lap-RFA, your doctor makes two small incisions in the abdomen to insert a slim viewing instrument (laparoscope) with a camera at the tip. Using the laparoscopic camera and a laparoscopic ultrasound tool, your doctor locates fibroids to be treated.
After locating a fibroid, your doctor uses a specialized device to deploy several small needles into the fibroid. The needles heat up the fibroid tissue, destroying it. The destroyed fibroid immediately changes consistency, for instance from being hard like a golf ball to being soft like a marshmallow. During the next three to 12 months, the fibroid continues to shrink, improving symptoms.
Because there's no cutting of uterine tissue, doctors consider Lap-RFA a less invasive alternative to hysterectomy and myomectomy. Most women who have the procedure get back to regular activities after 5 to 7 days of recovery.
The transcervical — or through the cervix — approach to radiofrequency ablation (Sonata) also uses ultrasound guidance to locate fibroids.
Laparoscopic or robotic myomectomy. In a myomectomy, your surgeon removes the fibroids, leaving the uterus in place.
If the fibroids are few in number, you and your doctor may opt for a laparoscopic or robotic procedure, which uses slender instruments inserted through small incisions in your abdomen to remove the fibroids from your uterus.
Larger fibroids can be removed through smaller incisions by breaking them into pieces (morcellation), which can be done inside a surgical bag, or by extending one incision to remove the fibroids.
Your doctor views your abdominal area on a monitor using a small camera attached to one of the instruments. Robotic myomectomy gives your surgeon a magnified, 3D view of your uterus, offering more precision, flexibility and dexterity than is possible using some other techniques.
Hysteroscopic myomectomy. This procedure may be an option if the fibroids are contained inside the uterus (submucosal). Your surgeon accesses and removes fibroids using instruments inserted through your vagina and cervix into your uterus.
Endometrial ablation. This treatment, performed with a specialized instrument inserted into your uterus, uses heat, microwave energy, hot water or electric current to destroy the lining of your uterus, either ending menstruation or reducing your menstrual flow.
Typically, endometrial ablation is effective in stopping abnormal bleeding. Submucosal fibroids can be removed at the time of hysteroscopy for endometrial ablation, but this doesn't affect fibroids outside the interior lining of the uterus.
Women aren't likely to get pregnant following endometrial ablation, but birth control is needed to prevent a pregnancy from developing in a fallopian tube (ectopic pregnancy).
Traditional surgical procedures
Options for traditional surgical procedures include:
Abdominal myomectomy. If you have multiple fibroids, very large fibroids or very deep fibroids, your doctor may use an open abdominal surgical procedure to remove the fibroids.
Many women who are told that hysterectomy is their only option can have an abdominal myomectomy instead. However, scarring after surgery can affect future fertility.
Hysterectomy. This surgery removes the uterus. It remains the only proven permanent solution for uterine fibroids.
Hysterectomy ends your ability to bear children. If you also elect to have your ovaries removed, the surgery brings on menopause and the question of whether you'll take hormone replacement therapy. Most women with uterine fibroids may be able to choose to keep their ovaries.
Morcellation during fibroid removal
Morcellation — a process of breaking fibroids into smaller pieces — may increase the risk of spreading cancer if a previously undiagnosed cancerous mass undergoes morcellation during myomectomy. There are several ways to reduce that risk, such as evaluating risk factors before surgery, morcellating the fibroid in a bag or expanding an incision to avoid morcellation.
All myomectomies carry the risk of cutting into an undiagnosed cancer, but younger, premenopausal women generally have a lower risk of undiagnosed cancer than do older women.
Also, complications during open surgery are more common than the chance of spreading an undiagnosed cancer in a fibroid during a minimally invasive procedure. If your doctor is planning to use morcellation, discuss your individual risks before treatment.
The Food and Drug Administration (FDA) advises against the use of a device to morcellate the tissue (power morcellator) for most women having fibroids removed through myomectomy or hysterectomy. In particular, the FDA recommends that women who are approaching menopause or who have reached menopause avoid power morcellation. Older women in or entering menopause may have a higher cancer risk, and women who are no longer concerned about preserving their fertility have additional treatment options for fibroids.
Comments
Post a Comment