General Discussion
Central diabetes insipidus (CDI) is a rare disorder characterized by excessive thirst (polydipsia) and excessive urination (polyuria). It is not related to the more common diabetes mellitus (sugar diabetes), in which the body does not produce or properly use insulin. CDI is a distinct disorder caused by complete or partial deficiency of the protein, arginine vasopressin (AVP), which is required by the kidneys to manage water balance in the body. If affected individuals do not have access to water, dehydration may occur. Eventually, more serious symptoms can develop including changes in consciousness and confusion associated with dehydration and elevation in serum sodium concentration (hypertonic dehydration). CDI may be caused by any condition that affects the creation, transport or release of vasopressin. CDI may be inherited or acquired. In some cases, no cause can be identified (idiopathic).
Symptoms
Signs and symptoms of diabetes insipidus include:
- Being extremely thirsty
- Producing large amounts of pale urine
- Frequently needing to get up to urinate during the night
- Preferring cold drinks
If your condition is serious and you drink a lot of fluids, you can produce as much as 20 quarts (about 19 liters) of urine a day. A healthy adult typically urinates an average of 1 to 2 quarts (about 1 to 2 liters) a day.
An infant or young child with diabetes insipidus may have the following signs and symptoms:
- Heavy, wet diapers
- Bed-wetting
- Trouble sleeping
- Fever
- Vomiting
- Constipation
- Delayed growth
- Weight loss
Causes of Central Diabetes Insipidus
Central diabetes insipidus results from a deficiency of vasopressin. The deficiency may be
Inherited
Caused by another disorder
Of unknown cause
Other disorders that can cause central diabetes insipidus include accidental damage done during surgery on the hypothalamus or pituitary gland; a brain injury, particularly a fracture of the base of the skull; a tumor; sarcoidosis or tuberculosis; an aneurysm (a bulge in the wall of an artery) or blockage in the arteries leading to the brain; some forms of encephalitis or meningitis; and the rare disease Langerhans cell histiocytosis.
Nephrogenic diabetes insipidus is another type of diabetes insipidus in which there is an adequate amount of vasopressin, but abnormalities in the kidneys cause them not to respond to vasopressin.
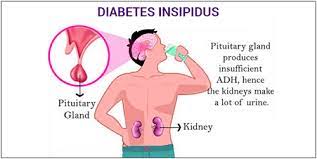
Central diabetes insipidus
In central diabetes insipidus, your body doesn’t make enough vasopressin, also called “antidiuretic hormone.” Vasopressin is produced in your hypothalamus, a small area of your brain near the pituitary gland. When the amount of fluids in your body falls too low, the pituitary gland releases vasopressin into your bloodstream. The hormone signals your kidneys to conserve fluids by pulling fluids from your urine and returning fluid to your bloodstream. But if your body can’t make enough vasopressin, the fluid may get flushed out in your urine instead.
Causes of central diabetes insipidus include
- damage to your hypothalamus or your pituitary gland from surgery, infection, inflammation, a tumor, or a head injury
- an autoimmune disorder
- an inherited gene mutation
- Nephrogenic diabetes insipidus
In nephrogenic diabetes insipidus, your body makes enough vasopressin but your kidneys don’t respond to the hormone as they should. As a result, too much fluid gets flushed out in your urine. Causes include
some medicines, especially those used to treat bipolar disorder NIH external link
- low levels of potassium in your blood
- high levels of calcium in your blood
- a blocked urinary tract
- an inherited gene mutation
- chronic kidney disease, though rarely
- Dipsogenic diabetes insipidus
In this type of diabetes insipidus, a problem with your hypothalamus causes you to feel thirsty and drink more liquids. As a result, you may need to urinate often. Causes include
damage to your hypothalamus from surgery, infection, inflammation, a tumor, or a head injury
- some medicines or mental health problems
- Gestational diabetes insipidus
Gestational diabetes insipidus is a rare, temporary condition that can develop during pregnancy. This type of diabetes insipidus occurs when the mother’s placenta NIH external link makes too much of an enzyme that breaks down her vasopressin. Women who are pregnant with more than one baby are more likely to develop the condition because they have more placental tissue.3 Because the liver plays a role in curbing the enzyme that breaks down vasopressin, diseases and conditions that affect liver function also increase risk. Examples include preeclampsia NIH external link and HELLP syndrome NIH external link.
Risk factors
Nephrogenic diabetes insipidus that's present at or shortly after birth usually has an inherited (genetic) cause that permanently changes the kidneys' ability to concentrate urine. Nephrogenic diabetes insipidus usually affects males, though women can pass the gene on to their children.
- Complications
- Dehydration
Diabetes insipidus may lead to dehydration. Dehydration can cause:
- Dry mouth
- Changes in skin elasticity
- Thirst
- Fatigue
- Electrolyte imbalance
Diabetes insipidus can cause an imbalance in minerals in your blood, such as sodium and potassium (electrolytes), that maintain the fluid balance in your body. Symptoms of an electrolyte imbalance may include:
- Weakness
- Nausea
- Vomiting
- Loss of appetite
- Muscle cramps
- Confusion
Diagnosis
Tests used to diagnose diabetes insipidus include:
Water deprivation test. While being monitored by a doctor and health care team, you'll be asked to stop drinking fluids for several hours. To prevent dehydration while fluids are restricted, ADH allows your kidneys to decrease the amount of fluid lost in the urine.
While fluids are being withheld, your doctor will measure changes in your body weight, urine output, and the concentration of your urine and blood. Your doctor may also measure blood levels of ADH or give you synthetic ADH during this test. This will determine if your body is producing enough ADH and if your kidneys can respond as expected to ADH.
Magnetic resonance imaging (MRI). An MRI can look for abnormalities in or near the pituitary gland. This test is noninvasive. It uses a powerful magnetic field and radio waves to construct detailed pictures of brain tissues.
Genetic screening. If others in your family have had problems with excess urination, your doctor may suggest genetic screening.
Treatment
Treatment options depend on the type of diabetes insipidus you have.
Central diabetes insipidus. If you have mild diabetes insipidus, you may need only to increase your water intake. If the condition is caused by an abnormality in the pituitary gland or hypothalamus (such as a tumor), your doctor will first treat the abnormality.
Typically, this form is treated with a synthetic hormone called desmopressin (DDAVP, Nocdurna). This medication replaces the missing anti-diuretic hormone (ADH) and decreases urination. You can take desmopressin in a tablet, as a nasal spray or by injection.
Most people still make some ADH, though the amount can vary day to day. So, the amount of desmopressin you need also may vary. Taking more desmopressin than you need can cause water retention and potentially serious low-sodium levels in the blood.
Other medications might also be prescribed, such as chlorpropamide. This can make ADH more available in the body.
Nephrogenic diabetes insipidus. Since the kidneys don't properly respond to ADH in this form of diabetes insipidus, desmopressin won't help. Instead, your doctor may prescribe a low-salt diet to reduce the amount of urine your kidneys make. You'll also need to drink enough water to avoid dehydration.
Treatment with the drug hydrochlorothiazide (Microzide) may improve your symptoms. Although hydrochlorothiazide is a type of drug that usually increases urine output (diuretic), it can reduce urine output for some people with nephrogenic diabetes insipidus.
If your symptoms are due to medications you're taking, stopping these medicines may help. However, don't stop taking any medication without first talking to your doctor.
Gestational diabetes insipidus. Treatment for most people with gestational diabetes insipidus is with the synthetic hormone desmopressin.
Primary polydipsia. There is no specific treatment for this form of diabetes insipidus, other than decreasing fluid intake. If the condition is related to a mental illness, treating the mental illness may relieve the diabetes insipidus symptoms.
Comments
Post a Comment